Ultrasound Leadership Academy: The Basics of Pelvic Transabdominal Ultrasound
Michael Macias
By Michael Macias
Welcome to the Ultrasound Leadership Academy (ULA) summary blog series. This week, we discuss the basics of pelvic (transabdominal) ultrasound. The ULA is essentially an online advanced ultrasound education experience put on by the team from Ultrasound Podcast which brings cutting edge learning to emergency medicine personnel through a variety of interactive platforms including video lectures, google hangouts with experts, simulation, live conferences and real time scanning with a pocket-sized ultrasound device known as a Vscan.
Over the next year I will be posting summaries of the key learning points from my experience. If you want to learn more about the program you can visit Ultrasound Leadership Academy or Ultrasound Podcast to see more from the hosts of this awesome program.
Prior to reading this post, I suggest you review our previous post "Introduction to Ultrasound" (including resource links at the bottom of the page) if you are not familiar with the basics of ultrasound.
INTRODUCTION
In the emergency room, we see a significant amount of female patients presenting with lower abdominal pain. Specifically, it seems that all too often it is located in the right lower quadrant, creating for us quite the diagnostic work up dilemma. Just as the urine pregnancy test has become a no brainer for initial work up of lower abdominal pain in a female, ultrasound is quickly becoming a point of care test that will likely be a close second in terms of
utility.
While there is robust literature on point of care ultrasound in pregnancy, the literature for non pregnant patients is still in development (a nice collection of pelvic-non pregnant ultrasound literature can be found at Sonospot here). I cannot definitely tell you that transabdominal pelvic ultrasound will drastically improve disposition time (we know it does in pregnant patients) or always be a diagnosis clincher, but with a test that is essentially free and can be performed in minutes, it is a scan well worth the effort, prior to ordering the CT scan, to assist in guiding your diagnostic work up in the right direction.
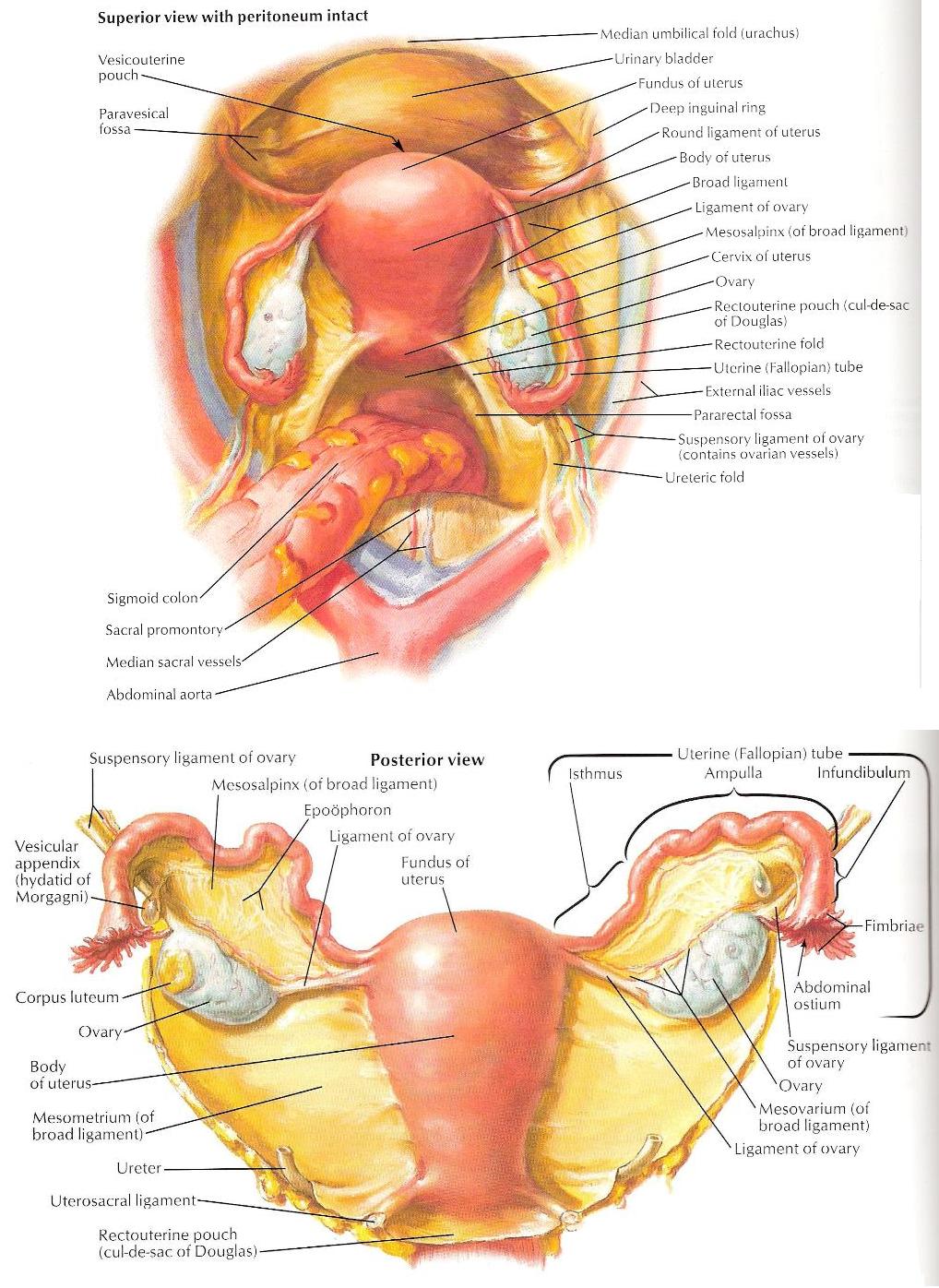
THE ANATOMY
The uterus is a pear shaped structure that lies directly posterior to the bladder and anterior to the sigmoid colon. It can further be broken down into a broad fundus, a tapering body, and a neck region known as the cervix. Its normal measurements after puberty are approximately 8 cm (L) x 5 cm (W) x 3 cm (D). The fundus often points anteriorly (anteverted) however it can also point posteriorly (retroverted) and can be flexed at the junction between the body and the cervix.
The fallopian tubes attach to the fundus of the uterus, supported by the well-named broad ligament. Their length averages 10 cm each. You will not be able to visualize the fallopian tubes on ultrasound usually unless they are enlarged secondary to fluid, blood or other pathology such as a tubo-ovarian abscess. Ovaries are usually ovoid in shape, and normal measurements are 4 cm (L) x 3 cm (W) x 2 cm (H). They are secured to the uterus by the ligament of the ovary and to the pelvic wall via the suspensory ligament of the ovary. The ovaries may be difficult to find on transabdominal ultrasound however notice their relationship to the external iliac vessels (usually anterior and medial) and use this relationship to guide your search.
THE TECHNIQUE
Probe: Curvilinear (low frequency) probe
Positioning: Supine. Be sure to drape appropriately and have the patient tuck the top of the cover sheet into the top of their undergarment to avoid getting gel on their clothes.
Location:
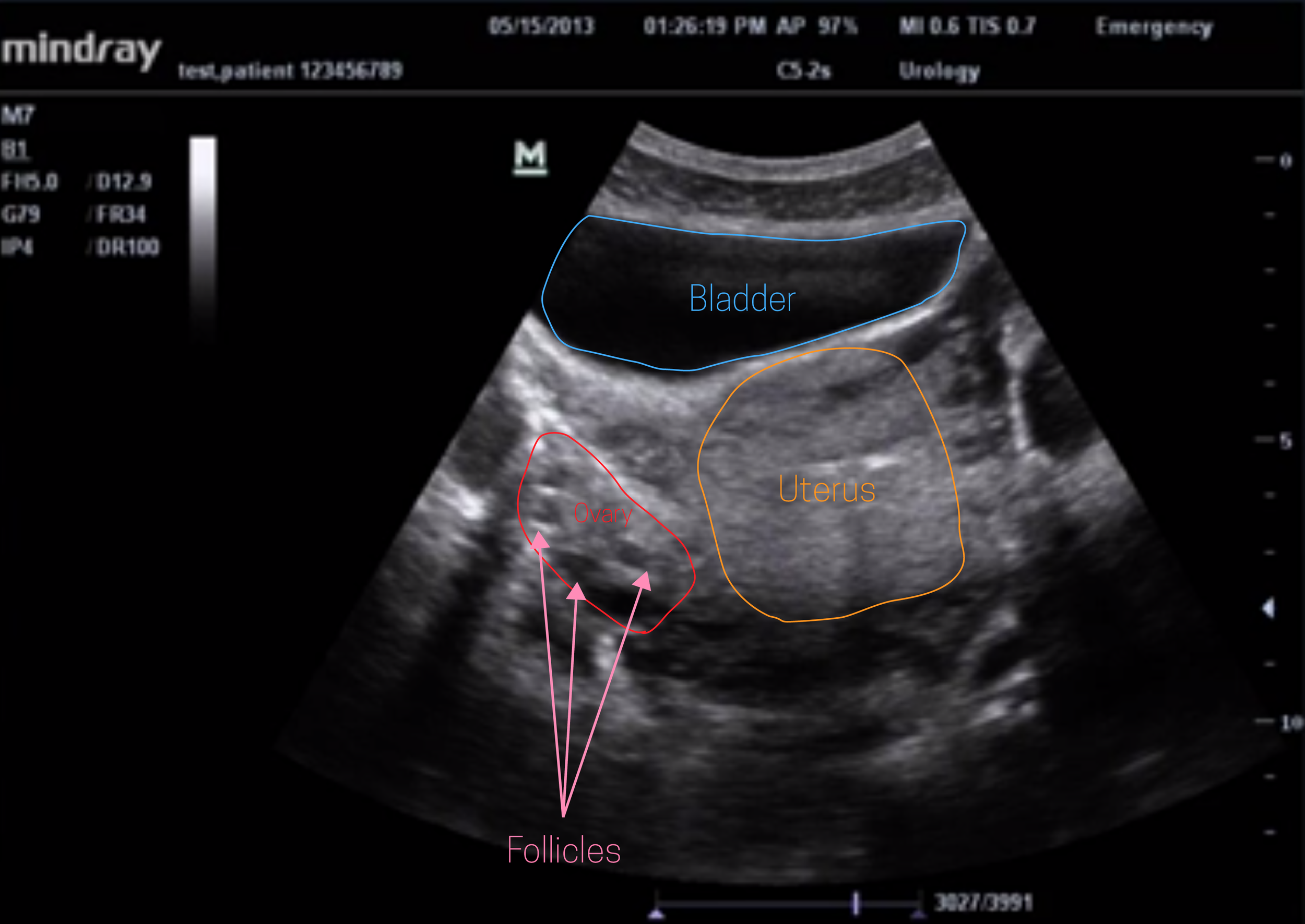
You are going to be scanning just above the pubic symphysis. It is very similar to the pelvic view of your FAST scan as you will be wanting to utilize the bladder as an acoustic window to view posterior structures (as well as displace bowel gas). Therefore a full bladder will significantly improve your scan and structure identification.
You will be obtaining both transverse and longitudinal views.
In the transverse view (with probe marker to patient's right), you will want to fan superiorly towards the fundus of the uterus as well as inferiorly until you visualize the lower uterine segment. You should also be able to visualize the vaginal canal which appears hypoechoic with a central hyperechoic region (vaginal stripe). Follicles (small hypoechoic structures) will aid in identifying the ovaries, though be sure to use color doppler to confirm as short axis view of blood vessels can appear similar.
Longitudinally, you will start midline, just above the pubic symphysis, and fan both left and right, examining the uterus, adnexa, and the posterior cul-de-sac (looking for fluid here). The endometrial stripe can be identified in this view as a hyperechoic line in the central uterus.
A PEEK AT PATHOLOGY
Cyst
Cysts will certainly be able to be identified on pelvic ultrasound, though sometimes will require a transvaginal approach. Cysts typically will appear anechoic (completely black), with thin walls and posterior acoustic enhancement. If the cyst is large (typically quoted measurement is > 4 cm) and the history is concerning for torsion, consider gynecologic evaluation and transvaginal ultrasound (even if color flow to ovary is visible).
Masses
Masses are not uncommon and you can be the one to pick up the diagnosis in an otherwise benign appearing patient. Masses may appear circular or ovoid but also can have quite irregular borders. They will be heterogenous and appearance will vary significantly depending on contents. Above note the dermoid cyst on the left. It contains both fat and fluid. The white arrowhead points towards echogenic fat while the white dashes you see represent hairs within the cyst. To the right is a large cystic structure behind the bladder with internal heterogenous echoes. Found in a patient with fever, nausea and cervical motion tenderness, this was eventually found to be a tubo-ovarian abscess that required drainage percutaneously.
Ovarian Hyperstimulation Syndrome (OHSS)
If you work near a fertility clinic you will at some point see this presentation. Woman who are receiving fertility assistance will often present after egg retrieval with a variety of symptoms from abdominal bloating and vomiting to significant shortness of breath. These patient can have significant third spacing of fluid including development of ascites, pulmonary edema and even pleural effusions. On pelvic ultrasound you will find significant free fluid as well as enlarged ovaries with multiple large and peripheral follicles. These patients are at risk for ovarian torsion.
I hope you enjoyed the quick rundown of transabdominal ultrasound in the non pregnant patient. We will cover the transvaginal scan as well as pelvic ultrasound during pregnancy in the near future so stay tuned. Here is a quick review of the scan as well as a few interesting cases:
- US Case: 15 y/o with fever and pelvic pain Sonospot
- US Case: 38 y/o with vaginal bleeding Sonospot
- US Case: Female with pelvic pain and a large mass EM Dutch
THAT'S IT FOR THIS WEEK
If you are interested in learning more about the ULA learning experience, visit their website below:
All images are courtesy of the ULA online video course unless otherwise stated. More on pelvic US can be found in "Introduction to Bedside Ultrasound," Volume 1 & 2, from Dr. Mallin and Dr. Dawson. If you are interested in purchasing these ebooks for less than $1, visit Ultrasound Podcast Consumables.